Multiple options for fentanyl treatment exist today. Choosing the right program involves understanding fentanyl addiction, how it works in the brain and body, why it’s crucial to seek treatment, and how to safely detox.
Anyone seeking treatment for fentanyl addiction must learn the necessary recovery skills to avoid relapses. This occurs through a combination of medication and therapy. Find out if you meet the criteria for fentanyl use disorder and discover the steps to take to get help.
Here you’ll get information about the following:
- How fentanyl compares to other opioids
- Why fentanyl abuse is a nationwide epidemic
- Signs and symptoms of fentanyl misuse
- Fentanyl withdrawal symptoms
- Various fentanyl treatment options and costs
This information will help you determine if you have a fentanyl use disorder and, if so, how and where to get the help you need and deserve.
What is Fentanyl and Why is It Unique?
Fentanyl is an opioid, like morphine and heroin. However, it’s a synthetic version that’s made in labs.
Doctors sometimes prescribe pharmacologic grade fentanyl for pain. However, most fentanyl is made and sold illegally, which makes it extremely dangerous and one reason why it causes so many deaths.
Pharmaceutical vs. Illicit Fentanyl
Pharmaceutical fentanyl is regulated and approved by the U.S. Food and Drug Administration. It can be taken through IVs, as lozenges or worn as topical patches.
Fentanyl created in clandestine labs is typically sold as powders, “M-30” pills, and analogs like car-fentanyl or acetyl-fentanyl. The street versions of fentanyl are often mixed with other drugs, such as benzodiazepines or xylazine, which makes them even more dangerous.
Potency
Fentanyl is 50 times more potent than morphine and 100 times more potent than heroin. Even those with a high tolerance for opioids can experience an overdose because a tiny amount of fentanyl, even just one pill, can kill. As few as two milligrams, equivalent in size to a few grains of salt, can be fatal.
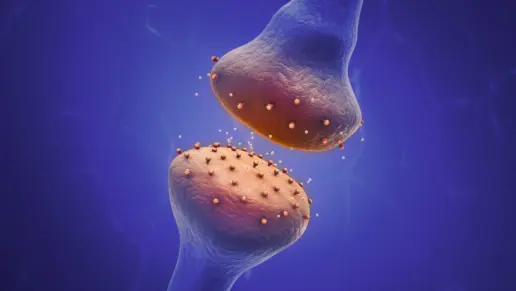
How Fentanyl Works in the Brain and Body
Fentanyl has a high lipid solubility. Upon being ingested, the drug enters the bloodstream and then the brain to change how the neurotransmitters, or feel-good chemicals, work.
It can cause a release of dopamine that’s much higher than what the brain can produce naturally. The release makes someone feel an intense rush, respiratory depression and euphoria.
As fentanyl leaves the system, the brain produces cravings to get high again. It can also create uncomfortable withdrawal symptoms. To avoid them and to satisfy cravings, users continue to take fentanyl. Over time, they may develop tolerance, dependence and addiction.
Fast-Growing Public Health Crisis
According to the Centers for Disease Control and Prevention (CDC) and the Drug Enforcement Administration (DEA), fentanyl is a fast-growing public health crisis and is involved in 70% of opioid overdose deaths. Despite a recent decline, fentanyl was responsible for over 70,000 overdose fatalities in 2023 and 48,422 in 2024.
Fentanyl was involved in 70% of opioid overdose deaths, according to the CDC and DEA.
70,000
Fentanyl overdose fatalities in 2023
48,422
Fentanyl overdose fatalities in 2024
The U.S. isn’t the only country seeing fentanyl-related problems. European and Latin American nations along with Australia are experiencing the impact of fentanyl’s presence. Numerous reasons contribute to this global epidemic.
How fentanyl enters the country has changed since its first arrival. Today, it comes from many regions. While China is still the primary source of fentanyl, Mexico and India are also now big trafficking routes. Unfortunately, how fentanyl enters the United States will continue to change and may increase.
In addition, counterfeit fentanyl and other drugs can be bought on social media platforms, which puts purchasers of all ages at significant risk. Many manufacturers are mixing xylazine with fentanyl. This “tranq dope” is attractive to many people with opioid use disorders because it allegedly prolongs their highs.
At-Risk Populations
Anyone who tries fentanyl is at risk for developing an addiction that can occur quickly. They’re also at risk of overdosing.
Among the populations most at-risk are:
- Teens wanting to experiment with fentanyl but are unaware of the dangers
- Chronic pain patients no longer receiving prescription pain medications
People who have polysubstance use disorders and take a mixture of fentanyl, benzodiazepines, and stimulants increase their risk of experiencing a lethal outcome. Fentanyl interacts adversely with many prescription and illicit substances.
Signs and Symptoms of Fentanyl Misuse
The signs and symptoms of fentanyl misuse vary for each person. However, common physical, psychological, and behavioral changes may occur, including:
- Drowsiness
- Confusion
- Pinpoint pupils
- Nausea
- Constipation
- Slower breathing
- Nodding in and out of consciousness
- Anxiety
- Depression
- Mood swings
- Intense cravings for more
- Hanging out with other drug users
- Financial troubles
- Decreased personal hygiene
- Missing prescriptions or running out early
- Doctor-shopping
- Isolating from friends and family
If someone runs out of fentanyl, is cut off from their prescription, or tries to quit using it cold turkey, they’ll likely experience severe withdrawal symptoms. To avoid withdrawals, they may continue using opioids or any other drug to ease their pain.
Fentanyl Withdrawal Timeline
Withdrawal symptoms may appear as soon as six hours after the last use of fentanyl. Having withdrawals is a sign of physical dependence on the drug.
Symptoms may include the following:
- Nausea
- Vomiting
- Excessive sweating
- Fever and chills
- Abdominal cramps
- Diarrhea
- Insomnia
- Muscle aches
- Runny nose
- Anxiety
Between 48 and 72 Hours
Symptoms can be severe and typically peak between 48 and 72 hours. They can be more intense than withdrawal from heroin or other opioids due to the drug’s shorter half-life and high affinity for the opioid receptors in the brain.
Overdose Warning Signs and Naloxone Response
Anyone using fentanyl must be aware of the overdose warning signs. Recognizing the signs and administering naloxone can save a person’s life from a fentanyl overdose.
Take action and call for help immediately if any of the following signs are present:
- Becoming unconscious or unresponsive
- Respiratory depression
- Central nervous system impairment
- Seizures or convulsions
- Flushed skin
- Extreme nausea or vomiting
- Agitation
- Hallucination
- Paranoia
- Blue lips
- Gurgling noises
Naloxone is a drug that can reverse a fentanyl overdose. Having naloxone near someone with a fentanyl use disorder is highly recommended at all times.
When an overdose occurs, administer 2 mg of naloxone every 2-3 minutes until it takes effect or until emergency responders arrive. Since fentanyl’s effects can outlast naloxone’s effects, the person overdosing needs rescue breaths and other CPR techniques as needed.
Self-Assessment
The Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition (DSM-5) lists 11 criteria to determine if someone has a fentanyl use disorder.
The 11 criteria are:
- Use more of the drug and for longer periods than intended
- Have intense cravings and urges
- Can’t quit using despite efforts
- Continue using even though it causes relationship problems
- Doesn’t stop even though it causes or worsens physical or psychological issues
- Keeps ingesting despite its interference with work, home, academic, or social responsibilities
- Spend much of the day seeking, using and recovering from fentanyl use
- Give up activities to spend more time using the drug
- Using fentanyl in hazardous situations or risky settings
- Developing tolerance
- Experiencing withdrawal symptoms
A mild addiction is meeting two or three of the above criteria. A moderate addiction is meeting four to five criteria, and severe is meeting six or more qualifications.
Another brief opioid-specific screener is the Tobacco, Alcohol, and Prescription Medication test. Additionally, some professionals utilize the Substances Tool (TAPS) and the Opioid Risk Tool (ORT).
Evidence-Based Treatment Pathway
For decades, evidence-based treatments have emerged to guide successful recovery journeys. Individual fentanyl treatment plans outline a path based on the severity of someone’s substance use disorder.
Medically Supervised Detox vs Social Detox
Medically supervised detox typically takes place in hospital or other inpatient clinical settings, where patients receive 24/7 supervision from doctors, nurses, and other medical professionals. They continually check vitals and administer medications like loperamide and clonidine to ease withdrawal symptoms.
Outpatient detox is another option for people with a lower risk of severe withdrawal or complications.
In this setting, a doctor prescribes medications to help manage symptoms, and the patient checks in regularly for monitoring. This approach allows people to stay at home and maintain some daily responsibilities while starting recovery.
Social detoxing is a non-medical approach to withdrawal management where individuals are monitored and supported in a residential or community-based setting without the use of medications to manage withdrawal symptoms.
Instead of medical interventions, the focus is on providing a safe environment, emotional support, hydration, nutrition, rest, and supervision by trained staff. It’s best suited for people who are unlikely to experience severe or life-threatening withdrawal symptoms.
Medication-Assisted Treatment (MAT)
MAT is very popular and effective in treating people with fentanyl use disorders. Medication is prescribed or administered to help ease cravings, prevent withdrawal symptoms and reduce the likelihood of a relapse.
Here are three examples of medications approved to treat fentanyl use disorders:
Buprenorphine
Buprenorphine binds to the mu-opioid receptors in the brain and blocks other opioids from attaching to those receptors. Buprenorphine eases withdrawal symptoms and is given in small clinical doses. Micro-induction may be used to reduce the likelihood of precipitated withdrawal when buprenorphine is started. Buprenorphine can be prescribed as a daily medication or as a monthly injected medication.
Methadone
Methadone reduces cravings and is the gold standard for severe opioid use disorders. It’s often taken for years to help someone maintain recovery. Methadone centers offer counseling, doctor check-ins, and clinical monitoring to ensure that any side effects, complications, or relapses are addressed..
Naltrexone
Naltrexone extended-release treatment begins after at least seven days of being opioid-free. It’s a fentanyl treatment option for someone with mild withdrawal symptoms, stable housing, and an excellent support system. It blocks the effects of opioids and reduces cravings for opioids.
Behavioral Therapies
Behavioral therapies are an essential part of a recovery plan. Those in treatment programs benefit the most when they combine medication with behavioral counseling. A person must learn early recovery and relapse prevention skills to ensure long-term sobriety.
Below are selected behavioral therapies effective in treating fentanyl use disorders:
- Cognitive behavioral therapy (CBT) teaches individuals to recognize triggers and craving cues, change negative thought patterns, and implement healthy behaviors.
- Dialectical behavioral therapy (DBT) is a form of CBT that teaches emotional regulation with a mindfulness aspect.
- Motivational interviewing (MI) helps someone who might not be fully ready to commit to recovery to see the benefits of no longer using drugs. It enhances readiness for change.
- Contingency management (CM) uses vouchers and rewards to encourage positive behaviors and help people reach milestones in recovery.
- reSET-O is a prescription digital therapeutic program used as an adjunct to taking buprenorphine. It offers CBT through a smartphone app.
Alternative and holistic therapies are available in most fentanyl treatment programs to aid recovery. They may include art, music, equine, sports, massage, meditation, yoga, and exercise that connect the mind, body, and spirit.
Levels of Care and Program Lengths
The American Society of Addiction Medicine has given specific codes for the various levels of care.
Here are some typical examples:
3.7
Medically Supervised Detox
3.5
Residential Rehab
2.5
Partial-Hospitalization Program
2.1
Intensive Outpatient Program
1.0
Outpatient Program
Evidence shows that those who spend 90+ days in combined inpatient and outpatient programs are more likely to remain sober after one year. Most programs for fentanyl addiction work as a continuum of care. People start at an intense level of care and step down to less intense services as they progress in recovery.
Special Populations
Certain groups of fentanyl users may need special programs during withdrawal and recovery. For example, babies born to women who start buprenorphine while pregnant may have neonatal abstinence syndrome (NAS). These newborns will need to be monitored after birth.
Adolescents taking diversion-proof buprenorphine films benefit from family therapies to ensure they get support at home during recovery. Many people who misuse fentanyl also have mental health disorders. Treating both disorders simultaneously is a must for recovery.
Continuing Recovery and Relapse Prevention
Recovery doesn’t stop when addiction treatment ends. It’s a lifelong process. Fortunately, fentanyl treatment centers offer ways to aid recovery and prevent relapses.
Aftercare Planning
Aftercare programs are individualized discharge plans that typically run for 30 days. They connect those leaving fentanyl treatment with community resources to help them maintain recovery.
Examples include:
- Sober living
- Outpatient therapy
- Peer support groups
- 12-step groups
- Job coaching
- Transportation
- Childcare
The aftercare plan can also include MAT refill scheduling, urine screens and counseling sessions. Each person has a unique plan tailored to their specific situation.
Peer and Family Support
Many families struggle with setting healthy boundaries and worry about enabling people with substance use disorders.
They also need help to overcome these behaviors and improve their overall well-being. Peer and family education and support may include attending Narcotics Anonymous (NA), SMART Recovery, or Recovery Dharma to learn different philosophical approaches to recovery.
Harm-Reduction Strategies
Harm-reduction strategies decrease the likelihood of fentanyl users experiencing overdoses or death. One method is to have naloxone on hand at all times. Naloxone should be given to anyone who spends time around the person using fentanyl. They should be given proper instructions on how to use it in life-threatening scenarios.
Fentanyl users can also benefit from safe-use education and from fentanyl testing strips to see if fentanyl is hidden in other drugs they may be taking.
Cost, Insurance, and Access
The cost of fentanyl addiction treatment varies due to many factors, such as location, insurance, services, and staff qualifications. Typical cost ranges include the following:
$300-$1000
$300-$1000 daily for detox
$300-$800
$300-$800 daily for inpatient
$100-$300
$100-$300 daily for outpatient
$5-$60
$5-$60 daily for MAT
Most insurance companies cover prescription medications and behavioral health treatment.
Anyone with the Affordable Care Act healthcare plans should be covered due to the Mental Health Parity and Addiction Equity Act. This law requires insurance to offer comparable services for people with mental health and substance abuse issues. Medicaid expansion specifically covers MAT in at least 40 states.
Even if insurance doesn’t cover the full cost, other payment options are available. Look up nonprofit scholarships, sliding scales, and Substance Abuse and Mental Health Services Administration (SAMHSA) grant-funded slots.
Recent policy changes help people get the fentanyl treatment they need. The 2023 MAT Act eliminated the DATA-2000 waiver and allows any medical doctor, nurse practitioner, or physician’s assistant with a DEA registration to prescribe buprenorphine.
In addition, the COVID-era telehealth flexibilities are extended through 2026. Both changes allow much greater access to treatment for fentanyl for people who might not otherwise have access to treatment.
Frequently Asked Questions (FAQs) About Fentanyl
Acute symptoms of fentanyl detox can last for up to a week. The first few days are the hardest. Milder withdrawal symptoms may linger for 3+ weeks, including protracted fatigue, depression, sleep-related issues, dysphoria or the inability to feel pleasure.
There are occasions when someone can taper off fentanyl successfully at home. However, most people require medical supervision and medications to help overcome unexpected health events, breakthrough cravings, relapse and overdoses. Getting away from an environment that can trigger relapses is essential during detox.
Precipitated withdrawal is the rapid onset of withdrawal symptoms due to taking buprenorphine while other opioids are already in your system. When given less than 12 hours from the last use of fentanyl, the risk of precipitated withdrawal is high with buprenorphine. Microdosing induction, including a regimen known as the Bernese method, can help.
MAT is given in clinical doses and is supervised by doctors and other medical staff. This creates more structure than relying on random doses for euphoric effects. Therefore, drugs like buprenorphine and methadone help stabilize brain chemistry. MAT lowers the risk of mortality by 50%-70%.
According to NIH HEAL initiative reports, researchers are developing a naloxone implant. This miniature overdose detection device automatically recognizes when the body overdoses. When a positive reading is detected, it releases naloxone into the system and notifies emergency responders. Although not yet been approved, the device can save numerous lives.
Find Fentanyl Treatment Near You
Before you search for “fentanyl treatment near me,” check out the online directory on Rehab.com to find fentanyl treatment centers. Use the filters to narrow your search by location, type of treatment program, insurance, treatment methods, and special programs or amenities.
If you aren’t sure where to start, call to talk to someone for help in connecting to a provider that treats fentanyl misuse or addiction. They can verify your insurance and address any questions you may have.
Call the number below to get help today.
Call A Treatment Provider
For a conversation about what treatment options are available to you.
Make a Call
Addiction Centers That Treat Opioid Addiction
Finding facilities near you…