Successful opiate addiction treatment combines medical detox, medication-assisted treatment, and therapy to create lasting recovery from narcotics.
This article explains how the opiate withdrawal process works, how FDA-approved medications such as buprenorphine, methadone, and naltrexone can help, and how cognitive behavioral and holistic therapies give you the tools you need to replace bad habits with positive ones.
You’ll learn how to choose the right level of care for your needs and see how insurance, Medicaid, or sliding scale plans can help pay for the cost of opioid rehab.
Don’t let opiates control your life for another minute. Read on to learn everything you need to know about treatment options for your unique situation and take the first step toward recovery today.
Key Points:
- Opiate addiction rewires brain receptors around pain and pleasure and is one of the most dependency-forming classes of drugs.
- Treatment for OUD begins with detox to manage withdrawal symptoms and side effects.
- Opiate withdrawal can last between 5 to 14 days, depending on the severity of addiction.
- FDA-approved medications like methadone, buprenorphine, or naltrexone are used to curb ongoing symptoms and cravings.
- Behavioral, holistic, and group therapies should be used alongside medication for best results.
- Private insurance, Medicaid, Medicare, and sliding scale options can help pay for opiate rehab.
What Are Opioids and Why are They Addictive?
Opioids are a class of natural, semi-synthetic, and synthetic pain relievers that attach to opioid receptors in the brain; their pleasurable dopamine surge can quickly create tolerance, physical dependence, and, for many, addiction.
When someone experiences pain, the brain produces natural opioids called endorphins. These bind to the receptors in the central nervous system (CNS) and reduce or inhibit pain signaling by stopping electric pulses in nerve cells.
Common prescription opioids like oxycodone and hydrocodone, as well as street drugs such as heroin or illicit fentanyl, act like super-charged endorphins. By latching onto mu-receptors, they block pain signals and release a wave of dopamine that the brain records as an intense reward.
Over time, the brain makes fewer natural endorphins and amplifies craving circuits, so a person needs higher or more frequent doses just to feel “okay.” When neurotransmitter levels drop too low, withdrawal symptoms flare up, driving compulsive use and creating a vicious cycle known as opioid use disorder (OUD).
In the U.S., opioid abuse has increased with devastating consequences, with widespread overdoses and a gap in addiction treatment received.
Nearly 70% of the 107,000 overdoses recorded in 2023 were due to opioids like Heroin and Fentanyl.
Only 25% of adults in the U.S. who needed treatment for OUD received it in 2022.
Opioids vs Opiates
Opiates and opioids belong to the same class of drugs and share a common mechanism of action. The main difference is that opiates are naturally derived forms of the drug, while opioids are synthetically produced in a lab.
There are three different types of opioids categorized by how they are made:
Natural opiates
These opiates occur in nature and are found within the seedpod of the poppy plant. Examples include morphine and codeine, both commonly used prescription painkillers.
Semi synthetic opioids
Oxycodone, hydrocodone, hydromorphone, and oxymorphone are examples of medications that combine naturally-occurring opiates and synthetic opioids. Heroin is an example of an illegal, semi-synthetic opioid made from morphine.
Synthetic opioids
Methadone, fentanyl, and propoxyphene are examples of opioids that are made in laboratories and recreate the effect of naturally-occurred opiates. Synthetic opioids can be made to be much more potent than their natural opiate relatives.
All opioids have a similar effect on the brain; however, a National Institutes of Health (NIH) study found that opioid drugs activate receptors in a location that is not affected by naturally occurring opioids. This different and more rapid interaction may help explain why opioid drugs have undesired side effects and lead to increased levels of tolerance, dependence, and addiction.
Common Opiates & Opioids
Opioids are used for a variety of purposes. Some of the most commonly used opioids are:
- Heroin: This illegal opioid is derived from morphine. It is highly addictive and dangerous. Street names for heroin include Black tar, H, Horse, Junk, Skag, and Smack.
- Fentanyl: The Drug Enforcement Administration (DEA) reports that fentanyl is 100 times more potent than morphine and 50 times more potent than heroin. Fentanyl is used for severe pain management through a skin patch during cancer treatment. Due to its strength, Fentanyl is often abused, manufactured illegally, and involved in a high percentage of overdose deaths involving opioids.
- Codeine: This opiate is naturally occurring and used to treat pain, coughs, and diarrhea. It is widely used in medications and combined with other painkillers such as co-codamol (codeine and paracetamol).
- Morphine: A natural opiate, morphine is used to treat severe pain and includes brands such as Duramorph, Avinza, Roxanol, and Kadian.
- Oxymorphone: Although it is derived from morphine, it is significantly more potent. It is used to treat pain or as an anesthetic and is prescribed under the brand name Opana.
- Oxycodone: This semi-synthetic opioid is derived from thebaine which naturally occurs in the poppy plant. Oxycodone is used to treat patients with moderate to severe pain. Brand names include Dazidox, Endocodone, Oxecta, Percolone, and Roxicodone.
- Hydrocodone: Hydrocodone is also made from codeine and often combined with acetaminophen and used for extreme pain relief. Medications containing this opioid include Vicodin, Anexia, and Lorcet.
- Hydromorphone: Prescribed under the brand name Dilaudid, hydromorphone is used as an effective painkiller that works quickly with potent sedative effects. Hydromorphone is two to eight times stronger than morphine. It is highly addictive and often abused.
- Buprenorphine: Another semi-synthetic opioid derived from thebaine. Buprenorphine treats opiate addiction as an opioid agonist-antagonist under brand names, including Suboxone, Subutex, and Buprenex.
Signs, Symptoms, & Risk Factors of Opioid Use Disorder
Opioids, like all drugs and medications, have side effects. When prescribed carefully by a medical practitioner and used accordingly, the benefit of taking the opioid will often outweigh the side effects, but they can become problematic when use increases in addiction.
The two most common side effects of opioid use are constipation and nausea. These side effects can be challenging to manage and continue throughout treatment. In some cases, it will be severe enough to require discontinuation of opioid use.
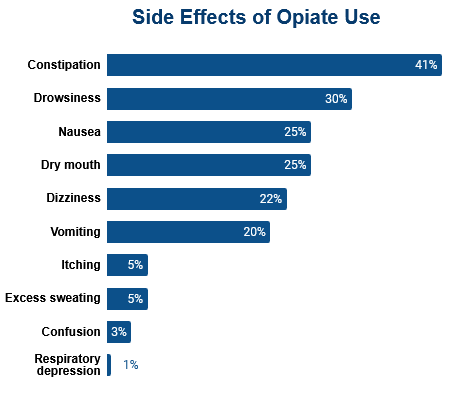
Other side effects are also possible, although they are less commonly experienced and are either temporary or easier to manage during treatment.
- Dizziness
- Vomiting
- Diarrhea
- Dry mouth
- Skin itching
- Slowed breathing rate
- Drowsiness
- Mood swings and irritability
How Do You Know if Someone Has an Opioid Addiction?
Some signs of opioid addiction to look out for include:
Continued use despite detrimental effect on health
Someone with an opioid addiction will likely be experiencing side effects and withdrawal symptoms, including constipation, nausea, and mood swings, but, despite this, they are unable to stop taking the drug.
Impact on relationships
When someone has a drug addiction, they may distance themselves from friends and family members due to fear of being judged or feeling shame.
Decreased social activities & declining performance
Opioid use disorder can cause a person to lose interest in or the ability to gain pleasure from things that they previously enjoyed. They have developed intense cravings and become fixated on sourcing and using more opioids.
Taking increasing doses of opioids
When someone uses opioids long-term, they develop a tolerance to their effects, meaning they need to take more of the drug to have the same effect.
Multiple opioid prescriptions from different clinicians
“Doctor shopping” is a common sign that someone is addicted to opioids. As most opioids require a prescription and their use is monitored, people who are addicted will often seek out multiple doctors to get multiple prescriptions for the same opioid.
Neglecting personal hygiene and appearance
Opioid addiction can lead to a noticeable decline in hygiene and grooming. Individuals may stop bathing regularly, wear dirty clothes, or appear generally unkempt, as drug use becomes their primary focus.
Who is at Risk of Becoming Addicted to Opioids?
With high prescription numbers and opioids being so addictive, it is easy to see why so many people develop a dependency and abuse them. The National Center for Drug Abuse Statistics states that 3.8% of American adults abuse opioids.
Anyone prescribed an opioid is at risk of addiction; however, some groups in society are more at risk than others. Risk factors for opioid abuse identified by the U.S. Department of Labor include:
- High dose: Those who have been prescribed a higher dose or a more potent opioid due to intense pain following an injury or operation are at higher risk for misuse and overdose death.
- Prolonged duration: Addiction to opioids can develop within a few days, and one in four people taking opioids long-term struggle with addiction. The American Society of Addiction Medicine published a guide called the National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. It is designed to provide doctors with information about the practical and responsible prescribing of opioids to reduce the chance of addiction.
- Extended-acting formulations: There is a greater risk of overdose and death with long-acting opioids such as morphine.
- History of alcohol or substance abuse: People with a history of addiction to other substances are more likely to become addicted to opioids. This should be taken into account when opioids are prescribed.
- Younger adults (18-25 years): Young people are at higher risk due to a family history of drug taking, childhood trauma, or a social or family environment that encourages misuse.
- Mental health concerns: People with depression, anxiety, bipolar disorder, or other mental illnesses are more at risk of developing an addiction. People use opioids for the euphoric effect to counteract the symptoms of their mental health condition.
Diagnosing OUD
The DSM-5 offers an 11-item checklist that helps clinicians determine whether someone’s opioid use has become a diagnosable disorder.
Each item captures a key warning sign, including frequent cravings, needing more of the drug to get the same effect, or continuing use despite problems at work or home.
During an assessment, the clinician reviews every sign in relation to the past year and notes each “yes,” giving a total score out of 11:
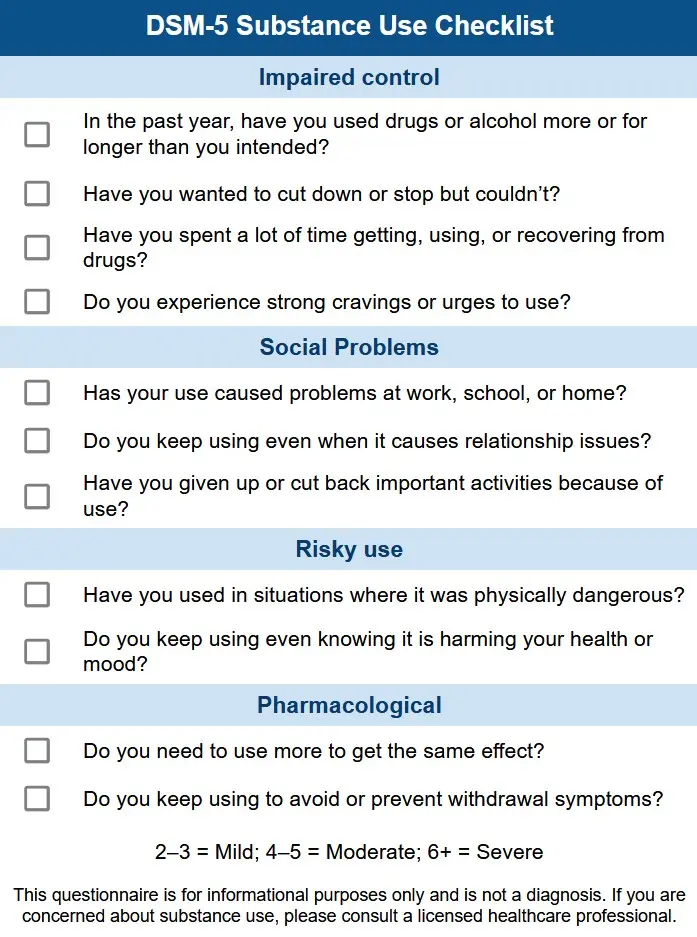
- 2 to 3 “yes” answers = mild OUD
- 4 to 5 “yes” answers = moderate OUD
- 6 or more = severe OUD
Take the self-assessment questionnaire now to see if you should consult with your healthcare provider about formal OUD testing.
If you still have questions you get answers 24/7 – call now to talk to someone about your or a loved one’s opioid addiction.
Call A Treatment Provider
For a conversation about what treatment options are available to you.
Make a Call
Why Professional Treatment Matters
If you think you might have OUD and need help, there are several reasons why you’ll want to consider finding good professional treatment.
Managing Withdrawal Symptoms
The time it takes for the withdrawal symptoms to start following the last dose depends on the opioid. For short-acting opioids like heroin, withdrawal symptoms can start within 8-24 hours and last for 4-10 days. For methadone and other long-acting opioids, withdrawal symptoms start within 12-24 hours and last for 10-20 days.
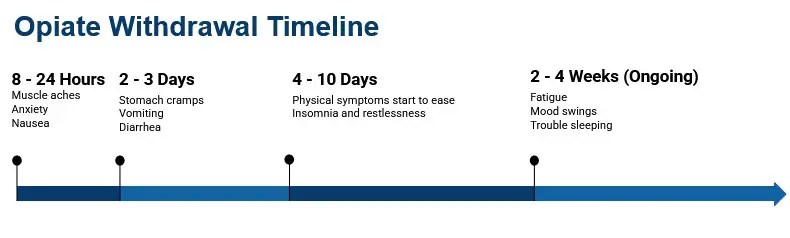
The symptoms of opioid withdrawal include:
- Nausea and vomiting
- Anxiety
- Insomnia
- Hot and cold flushes
- Perspiration
- Muscle cramps
- Watery discharge from eyes and nose
- Diarrhea
Evidence-Based Care vs. “Cold Turkey”
Quitting opioids abruptly (“going cold turkey”) may sound faster, but it shocks the nervous system and triggers severe withdrawal that can sap motivation, spike relapse risk, and raise the odds of a fatal overdose if a person returns to prior doses.
In contrast, evidence-based treatment uses medically supervised tapering, FDA-approved medications, and round-the-clock monitoring to keep symptoms manageable and vital signs stable.
These medications occupy opioid receptors just enough to calm cravings and prevent painful detox symptoms without producing the intense high that drives misuse. When combined with counseling, peer support, and relapse-prevention planning, they cut overdose deaths by up to 50 percent and nearly double long-term recovery rates compared with unsupervised withdrawal.
Professional programs also screen for co-occurring mental health or chronic-pain issues, adjust dosing over time, and create personalized aftercare plans.
Evidence-Based Treatment Options
The next step is understanding your treatment options: picking an appropriate level of care, choosing the right medication, and other therapies and specialty programs you may want to look for.
Levels of Care
Opioid recovery moves through standard levels of care, matched to your symptoms and schedule:
- Medical detox: 24/7 or clinic oversight eases withdrawal and starts stabilizing meds.
- Residential rehab: Live in care that blends counseling, MAT tweaks, and relapse-prevention practice.
- Partial Hospitalization (PHP): Daytime therapy 5 to 6 days a week; home at night while clinicians refine your plan.
- Intensive Outpatient (IOP) & standard outpatient: Evening or weekend groups taper to quick check-ins so you can work or study.
- Tele MAT: video sessions that can deliver buprenorphine renewals, online counseling, and remote drug screens.
Medication-Assisted Treatment (MAT)
MAT programs combine counseling with FDA-approved medications that calm cravings, protect against relapse, and cut overdose deaths in half, giving people with opioid use disorder the biological stability they need to focus on recovery.
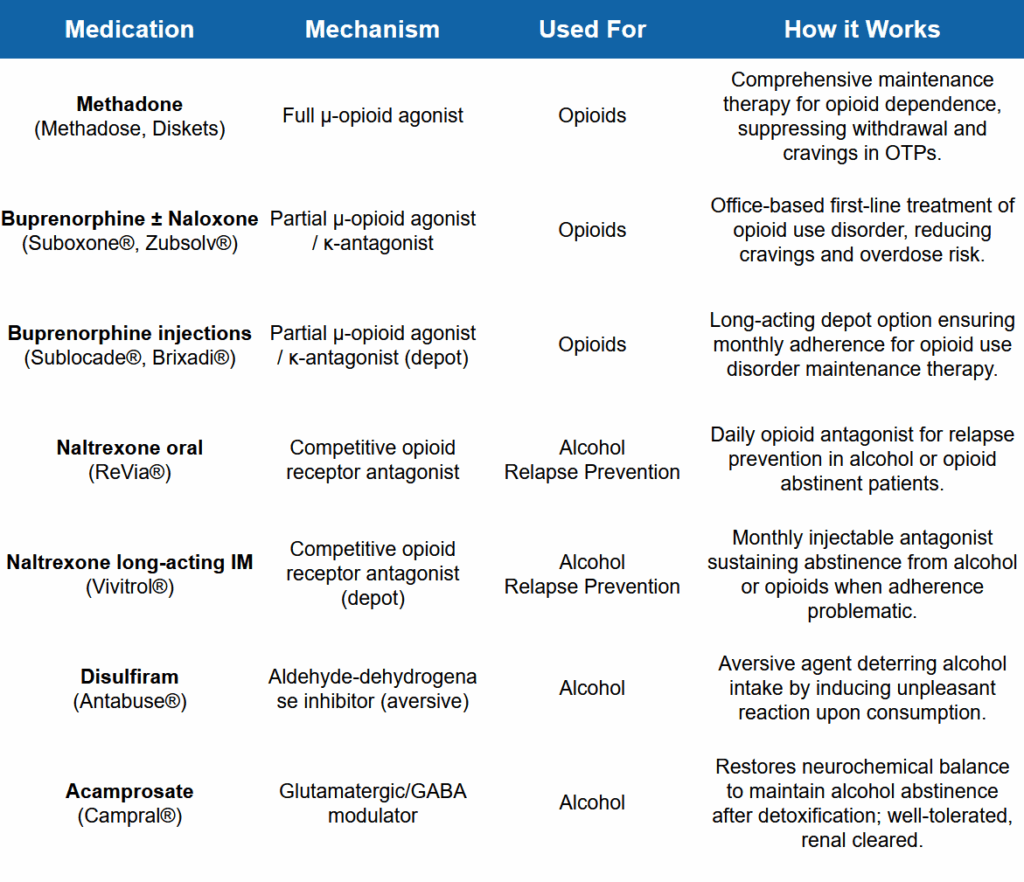
Common medications used in opiate treatment include:
- Methadone: A full agonist taken once daily at specialized clinics; steady blood levels curb withdrawal and are the gold-standard for pregnancy because they lower fetal stress.
- Buprenorphine (Suboxone): A partial agonist available in office-based or telehealth settings; its “ceiling effect” limits misuse while allowing most patients take home dosing and normal work routines.
- Naltrexone (Vivitrol): A non-addictive, monthly injection that blocks opioid receptors after detox; ideal for highly motivated individuals or those unable to visit a clinic regularly.
Long-term studies show 12-month retention rates of 50 – 60 percent with methadone and about 45 percent with buprenorphine, compared to under 15 percent for medication-free approaches.
Behavioral & Holistic Therapies
Evidence-based talk therapies reset thought patterns and boost coping skills. Cognitive Behavioral Therapy (CBT) tackles triggers directly, Dialectical Behavior Therapy (DBT) adds emotional regulation tools, Motivational Interviewing strengthens readiness for change, and contingency management pairs healthy actions with tangible rewards.
Because many people self-medicate trauma, programs layer in Eye Movement Desensitization and Reprocessing (EMDR) or Seeking Safety to reduce flashbacks and high-risk behaviors.
Holistic treatment programs such as guided mindfulness, tailored exercise plans, balanced nutrition, and structured family therapy can also help stabilize mood, strengthen positive habits, and improve overall recovery.
Special Considerations & Co-Occurring Needs
Dual Diagnosis (Mental Health)
Opiate recovery succeeds more often when depression, anxiety, PTSD, or other co-occurring mental health disorders are treated at the same time. This kind of integrated care lowers relapse risk and improves treatment success rates.
These programs start with a dual diagnosis assessment, then add in psychiatric medication management alongside traditional opiate MAT treatment. Psychiatrists and addiction specialists coordinate to avoid drug-interaction pitfalls and to fine-tune dosing so mood stabilizers, SSRIs, or antipsychotics support, rather than hinder, withdrawal progress.
Therapies such as trauma-informed CBT or EMDR address the underlying emotional pain that often fuels opioid cravings, while peer groups normalize talking about mental health in recovery. Discharge planning links clients to outpatient counseling, telepsychiatry, and supportive housing. These are important steps for individuals whose symptoms can flare under stress and trigger a return to use.
Specialty Populations
Opiate treatment is not one-size-fits-all; specialized drug rehab programs keep vulnerable groups safe while allowing clinicians to focus care on specific populations.
- Women & pregnancy: Prenatal methadone or buprenorphine, coupled with OB-GYN oversight, prevents fetal stress and supports healthy deliveries.
- Adolescents: Youth-focused programs weave family therapy and school coordination into shorter, developmentally tuned sessions.
- Older adults: Geriatric dosing guards against falls and interactions with common heart or diabetes medications.
- LGBTQ+ community: Affirming counselors reduce stigma, boosting engagement and mental-health stability.
- Re-entry programs: Jail-to-community MAT handoffs cut post-release overdose deaths.
- Rural & underserved areas: Mobile clinics and telehealth bridge “treatment deserts,” delivering buprenorphine and counseling by video.
- Veterans & first responders: Trauma-informed care addresses PTSD and moral injury.
- Chronic pain patients: Integrated pain clinics combine non-opioid therapies, physical rehab, and careful MAT titration to manage discomfort without relapse
Preparing for & Paying for Treatment
Taking the next step is easy. Here’s what you can expect if you’re ready to seek professional inpatient treatment for your opiate use.
Admissions Process & What to Expect
Here’s a brief overview of what you can expect from inpatient rehab programs from start to finish:
- The first step is a pre-assessment at a local drug rehab. This is usually a 20-minute phone or telehealth screening that reviews medical history, insurance details, and substance-use patterns.
- A nurse then creates a personalized withdrawal timeline so staff know when cravings or flu-like symptoms may peak.
- Pack light: bring a photo ID, insurance card, comfortable clothing, closed-toe shoes, current prescriptions, and a list of important phone numbers. Leave valuables, aerosols, and unsealed OTC meds at home.
- On arrival, a clinician performs lab work and a mental health check before assigning a room and introducing you to your care team.
- Typical length of stay runs 3 to 7 days for medical detox and 28 to 45 days for residential rehab, but every plan adjusts to progress and co-occurring needs.
- Discharge isn’t the finish line; case managers line up aftercare such as intensive outpatient, tele-MAT refills, sober housing, or alumni meetings to keep momentum strong.
Cost & Insurance
Most private insurers cover opioid treatment thanks to mental-health parity rules, though you can still expect to pay a deductible or co-pay. The exact amount of payment will vary between providers.
Below are average self-pay costs per day so you can compare options apples-to-apples:
- Medical detox: $300 to $1,000 per day, typically 3 to 7 days.
- Inpatient residential rehab: $300 to $800 per day for a 30-day stay in a private facility.
- Outpatient: $100 to $300 for each clinic day, depending on treatments and therapies needed.
Medication-Assisted Treatment (MAT) treatment for ongoing maintenance is generally more affordable (keep in mind these are approximate averages):
- Methadone maintenance: $18/day
- Buprenorphine/Suboxone: $16/day
- Naltrexone (Vivitrol) injection: $40/day
If the cost of treatment seems daunting, Medicaid, Medicare, and many state grant programs pay for methadone, buprenorphine, and counseling in certified clinics.
Sliding scale fee programs and scholarships help if you don’t have private health insurance coverage. Rural residents can use telehealth subsidies and veterans and pregnant women often receive priority funding.
Don’t let the cost of treatment prevent you from getting the care you need. Talk to someone today to verify your benefits and explore your treatment options.
Call A Treatment Provider
For a conversation about what treatment options are available to you.
Make a Call
FAQs & Helpful Resources
What’s the difference between opioid dependence and addiction?
Dependence is a physical state where your body adapts to the drug and experiences withdrawal if you stop suddenly. Addiction (opioid use disorder) adds a behavioral layer: compulsive use despite harm, cravings, and loss of control.
You can be dependent after legitimate pain therapy without being addicted, but untreated dependence can evolve into full addiction over time.
How long will I need to stay on buprenorphine or methadone?
Everyone’s timeline of recovery from opiate addiction is different. Research shows that staying on medication for at least 12 months sharply reduces relapse, yet many people continue maintenance therapy for several years with gradual dose adjustments.
The right taper schedule balances brain chemistry healing, life stressors, and personal goals, always under medical supervision to prevent relapse and overdose risk.
Do fentanyl test strips or naloxone belong in a treatment plan?
Absolutely. Harm reduction tools like fentanyl test strips help people who still use opioids detect deadly adulterants, while naloxone (Narcan) reverses overdoses in seconds.
Even after entering recovery, keeping naloxone on hand protects you and your community; many programs train clients and families so that swift intervention can turn a crisis into a second chance.
How can family members best support someone in opiate treatment?
Consistent, non-judgmental encouragement is key. Attend family education sessions, learn the signs of relapse, and practice healthy boundaries to support without enabling.
Joining groups like Al-Anon, SMART Family & Friends, or local peer-support meetings provides space to process your own emotions and learn practical strategies that reinforce your loved one’s recovery plan.
Is “rapid” or anesthesia-assisted detox a safe shortcut?
While marketed as a quick fix, putting someone under anesthesia to flush opioids from the body carries anesthesia risks, doesn’t erase cravings, and lacks the counseling component proven to sustain recovery.
Most experts recommend evidence-based medical detox followed by medication-assisted treatment and therapy – an approach with decades of safety and outcome data behind it.
Find Opiate Treatment Programs
Ready to act? Explore our nationwide rehab directory to find the best opioid rehab centers near you, and filter by insurance accepted, levels of care offered, and more. With a few clicks you’ll see detox, MAT, and outpatient options that match your medical needs and lifestyle.
Prefer one-on-one guidance?
Call
800-985-8516
( Sponsored Helpline )
today to speak to someone who can verify benefits, explain medication-assisted treatment programs, and schedule a same-day assessment.
The moment you reach out, you open the door to healing, stronger relationships, and a future free from opioid misuse. Take the first step today; your recovery journey can start right now.
Addiction Centers That Treat Opioid Addiction
Finding facilities near you…





