

Addiction Treatment for Veterans: Detox, PTSD, and VA Benefits
Specialized alcohol & drug rehab programs for veterans provide addiction treatment that understands military culture, PTSD, chronic pain, and the challenges of coming home. Explore how to find the best addiction treatment for veterans, what to expect from detox through aftercare, and how VA, TRICARE, and community programs can help you or a loved one start healing.
Best Alcohol & Drug Rehabs for Veterans
| Name / Address / Rating | Description | Treatments / Payments / Programs | Review / Contact | Images |
|---|---|---|---|---|
Cave Creek, AZ 1
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.90 / 10 | Soberman’s Estate, located in Cave Creek, Arizona, is an alcohol and drug rehab center that provides addiction treatment services to adult men, professionals, and public figures. They are a discrete, luxury rehab for individuals aged 30 to 80 years old. This location caps their treatment center at ten men at a time. As one of leading inpatient re | Treatments Programs Payment Options | Soberman’s Estate was everything I needed for my recovery. The staff, the program, physical activity and culinary experience were top notch and essential. The program is well designed and worked better than I expected. The staff is remarkable – professional, considerate and genuinely caring. My time there and being removed from alcohol for five weeks was everything I needed to remove my craving for alcohol. Soberman has changed my life in ways I never could have imagined. I feel confident, secure and grateful for my new life. I have reconnected with my family and friends. Thank you Soberman.
George B.
3 months ago
Yes, very professional staff, treatment, therapist, chefs were good! even the home cook did the best she could, and loved the horses of Course! Saturday morning hiking was fun to explore the trails of the nearby mountain area!
John E Williams
4 months ago
I had a great experience overall and would recommend it to anyone wanted to jump start their sobriety!!
Kevin Crawford
4 months ago
| 
5 5 



|
Clarksville, IN 2
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.81 / 10 | Avenues Recovery Center in Clarksville, Indiana, is an inpatient drug and alcohol detox and rehab center. They strive to provide individuals receiving treatment with a loving environment and attentive medical care. You’ll be away from toxic environments and triggers and have the opportunity to focus on developing life skills that will support you | Treatments Programs Payment Options | I highly recommend Avenues. The staff is absolutely amazing and very helpful. They treat you like family. Star, Jenny, Tarah, Paige, Monica, and both Amanda’s really helped me through.
Dana Key
3 weeks ago
It was a great experience great people thank you .
Jessica Fulkerson
3 weeks ago
This facility has been life saving. I am so grateful to be able to have gotten the help they had offered.
Nikki
3 weeks ago
| 
4 


|
Simi Valley, CA 3
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.81 / 10 | All In Solutions Detox in Simi Valley is one of the best ranked inpatient detox facilities in California providing safe, medically supervised care for individuals beginning their recovery from drug or alcohol addiction. As part of the All In Solutions Behavioral Health network, this facility serves as the first step in a full continuum of care. Cli | Treatments Programs Payment Options | I had an amazing experience and really enjoyed getting to know the staff and my fellow peers in groups. The staff really cares about your recovery and you will feel better every day. The food is good too lol.
Desiree
1 week ago
I loved it here it was a great place to be would definitely recommend to anyone wanting to get sober thank yall!
Kyle Robinson
1 week ago
i owe it all to this place. 100% recommend if you’re serious about your recovery. thanks AIS ❤️
maddy chacos
1 week ago
| 
5 5 



|
Hurst, TX 4
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.80 / 10 | Symetria – Hurst Outpatient Rehab and Suboxone Clinic in Hurst, Texas, is a private drug rehabilitation clinic for adults. One of the best outpatient rehab centers in Texas, Symetria offers various withdrawal medications to help clients get started with their recovery journey. You’ll also have access to treatments such as the intensive outp | Treatments Programs Payment Options | Symetria is unbelievably amazing!!! The Hurst staff is phenomenal!!! I can’t imagine that another location has a better staff. A special shout out to Deborah, Benjamin, and Samantha of course. You all are doing amazing, amazing, selfless work. You all are very special to so many!!!
Vernon Godsey III
3 months ago
Huge shout out to the team at symetria who make me feel like family I appreciate everything they do and huge shout out to Osagie for helping me! He is AWESOME!!! I love you symetria❤️❤️❤️
Chloe Roseman
4 months ago
BEST PLACE EVER. I have tried various other doctors/clinics and none of them even begin to compare to this one. The staff here is absolutely amazing. I can’t even make a single complaint. Dr Son is the best as well. He explains everything and you truly feel like he understands you. I can proudly say this, this place saved my life. If you or someone you know needs help getting off opiates do it right the first time and come here. You won’t be disappointed. If you are specifically struggling with fentanyl please don’t waste your time with other ways. I have tried 6 other methods from lazer therapy to having the earpiece to suboxone. Methadone is the key to our current fentanyl crisis. This clinic makes recovery possible again!
Mason
4 months ago
| 
5 5 



|
Boynton Beach, FL 5
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.80 / 10 | All In Solutions Counseling Center is a mental health center and addiction treatment program in Boynton Beach, Florida. They provide a partial hospitalization program, an intensive outpatient program (IOP), an outpatient program, medication-assisted treatment, and mental health care for adults with substance use disorder. All In Solutions Counseli | Treatments Programs Payment Options | The staff were amazing. Can really tell the people care about you. Amazing people who have lived through the experience and recovery they are trying to show all of us. Can’t recommend it enough.
Tyler
1 week ago
such a good facility. love all the staff! nicole is an awesome therapist!
Sydney Shaw
1 week ago
All In Solutions received me with open arms for the second time. The staff make sure you receive a high quality care treatment. I’m grateful for the love and care . God continue to bless everyone.Thank you for you do .
Jianil Richiez
3 weeks ago
| 
4 



|
Galloway, NJ 6
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.80 / 10 | Boca Recovery Center – Galloway is a drug and alcohol rehab in Galloway, NJ. They provide inpatient addiction treatment and medical detox. Boca Recovery’s New Jersey Drug & Alcohol Rehab, located in Galloway, New Jersey offers residential addiction treatment, medical detox, and medication-assisted treatment in an immersive treatment s | Treatments Programs Payment Options | My sobriety journey started at Boca. The staff members including Miss Tracey, Hannah and Kevin their alumni coordinator have completely flipped the trajectory of my life. I was immediately taken in with open caring arms and they made my detox process as comfortable as possible. During my stay, Joe was extremely helpful in helping me slowly gain my appetite back and start to feel stronger and was so attentive to my nutritional health. Nurse Patrick was so kind to me during my intake and Kevin still reaches out to me very often to check in and is so helpful in my recovery process. I owe gaining my life, my strength and my family back to Boca and I am eternally grateful❤️
Rianna Dean
1 month ago
Great facility with even greater staff. One of the best rehab/detox in South, NJ.
Donna Kratzer
1 month ago
Very comfortable stay
Will
1 month ago
| 
7 7 



|
Bloomington, IN 7
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.78 / 10 | The Boca Recovery Center is a luxury alcohol and drug rehab center for adults in Bloomington, Indiana. They specialize in cutting edge addiction treatment provided in a residential setting. One unique part of this alcohol and drug rehab in Indiana is the peaceful, secluded setting. If recovering in a clinical hospital setting doesn’t sound very a | Treatments Programs Payment Options | This place damn near saved my life. Staff is amazing and care almost on a personal level. Nurses are knowledgeable and groups are interactive informative and inclusive.
Edit*
Shout out to Beth, Nora and Carter! Made a great impact on my recovery!
V Montez
1 week ago
I learned a lot from this place. They’re really good at bringing everything out that you need to say in under to recovery. Thanks for everything. You guys have changed my life
Megan Tipton
2 weeks ago
Boca recovery was a magical experience during a very difficult time that will always hold a special place in my heart. From top to bottom, the support of staff is second to none.
Tyler and Carrie, Carter, Alexx, Ashley, Brooke, Michelle, Meagan, and the rest of the techs are phenomenal. My therapist January opened my eyes to perspectives I had been missing my entire life and Justin the case manager worked tirelessly from the start all the way until his wife gave birth on my last day to make sure I was set up for success.
The nurses are amazing and the medical attention someone needs during this portion of their recovery is 110% offered around the clock.
The place has everything you need from a gym to recreational activities, spacious beds with luxury amenities. And one cannot go without mentioning the chef, Tim. You won’t find better “rehab food” and conversation.
I owe a thank you to the director John for his efforts to get me into a great program after my stay was over.
To anyone struggling with with mental health and/or addiction, I cannot shout praises loud enough for what this program has to offer each and every client that walks through those doors.
If you want a way out, there’s no better place to check in.
Alex K
1 month ago
| 
6 6 



|
Woodbury, TN 8
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.77 / 10 | If you’re looking for a Christian-based men’s drug rehab center, S2L Recovery in Woodbury, Tennessee, might be the place for you or your loved one. Located at the top of Short Mountain, and overlooking the green hills of Middle Tennessee, this residential and detox clinic boasts a one-to-one staff/patient ratio so there’ll always be someone t | Treatments Programs Payment Options | Coming from Canada, I was hesitant. But God knew that S2L was exactly where I needed to be. At 64 years of age, I was able to discover my true identity, purpose, and mission in Christ. They help you in trying to get clean and sober for sure. But what S2L and the staff are all about is the Gospel of Jesus Christ. That’s why it is so successful.
TIM TANNER
4 months ago
I’ve had the privilege of seeing the life-changing impact this ministry has on countless men & I can’t recommend it highly enough! God has His Hand on this ministry & I’m honored to see the Lord work in these men!
Hunter Stanfield
4 months ago
Come here with a open mind and heart. It can and WILL change your life in all ways. Trust the process and trust God! Could go on and on about how amazing this place, I’ll forever be grateful!
Trevor Woodard
4 months ago
| 
6 6 



|
Levittown, PA 9
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.76 / 10 | The Steps To Recovery addiction treatment center is situated in Levittown, Pennsylvania. At this drug rehab center, patients can expect to engage in a unique treatment approach that focuses on helping individuals recover through authenticity, intimacy, community connection, and transparency. Steps to Recovery offers a serene and private environ | Treatments Programs Payment Options | Good place, great housing
Nicole Rivera
2 months ago
Amazing support network and great staff lovely time with my stay at STR buck
William Perry
3 months ago
My experience at Steps to Recovery has been great for the most part, the people and the environment are very welcoming and comforting. I have had some issues that have come up, but they usually get resolved. My only main gripe is with some of the other clients at the community living house fail to clean up after themselves, and some do not know self control. But, the staff here is very professional and easy to talk to. I find that the opportunities here for my recovery journey are pretty good, although I’d like access to more holistic therapy resources. I’ve actually personally facilitated a Dharma meeting and will facilitate more in the future. I appreciate my time here at STR and am excited for the future with them.
Jerry Davis
3 months ago
| 
6 6 



|
Watsonville, CA 10
Top 10 in Military Program
Rehab Score
Our Rehab Score is designed to make it easier for you to find the best treatment centers. We combine overall ratings with recent feedback to create a score that reflects a center’s quality right now.
8.76 / 10 | Located in Watsonville, California, Elevate Addiction Services provides alcohol and drug rehab services to men and women suffering from addiction. Their levels of care include detox, inpatient treatment, and outpatient treatment. One of the best ranked Outpatient treatment centers in California, Elevate Addiction Services provides a wide continuum | Treatments Programs Payment Options | Elevate was an awesome experience. I learned a lot about myself and I now have the tools for long term sobriety
Colin Yan
6 days ago
Elevate has been a life changing experience. The staff is very professional and compassionate. The community of clients is very special and the morale is unlike anywhere else. I would highly highly recommend Elevate Addiction Services to anyone struggling with addiction. From detox to the very end of your stay you are well taken care of.
Travis Boe
6 days ago
I have been through other treatment facilities in the past; but Elevate has by far been the best experience I could’ve hoped for. Recovery isn’t just the ability to abstain from substances, but the capability of transforming from within. Not only has Elevate help me appreciate the things within me but everything around me as well. Thank you, Elevate for changing the trajectory of my life and my marriage!!
Michael Amodeo
1 month ago
| 
5 5 



|

Challenges of Addiction Treatment for Veterans
Challenges of Addiction Treatment for Veterans
Veterans face unique challenges that can increase the risk of substance use disorders (SUD), from combat trauma and moral injury to chronic pain and isolation after separation from the Armed Services. Addiction treatment tailored for veterans and military culture is essential for effective recovery.
Let’s explore the data, common substances misused and co-occurring conditions and available therapies used to improve the quality of life for veterans. We also outline the levels of care in rehab, access points through the VA and community programs and financial resources to help veterans reclaim their health.
Key Facts About Drug Rehab for Veterans
Roughly 1 in 10 post-9/11 veterans meet criteria for substance use disorders; heavy drinking is highest in the Marine Corps and Air Force.
Post traumatic stress disorder (PTSD), moral injury, traumatic brain injury (TBI), military sexual trauma (MST), and chronic pain significantly increase relapse risks and complicate treatment planning.
VA and community programs offer inpatient, outpatient, teletherapy, and sober-living options tailored to veterans’ needs.
Evidence-based therapies include cognitive processing therapy (CPT), EMDR, acceptance and commitment therapy, peer mentorship and holistic wellness models.
VA benefits, TRICARE, grants, and scholarships can reduce or eliminate out-of-pocket rehab costs.
Relapse prevention, peer support and vocational resources support long-term recovery after discharge.
Addiction in Veterans and Military
Addiction in Veterans and Military
Substance Abuse in Veterans
Approximately 1 in 10 post‑9/11 veterans meet criteria for a substance use disorder (SUD), with alcohol misuse being most common. Heavy drinking is notably higher in the Marine Corps, followed by the Air Force, the Army, and then the Navy.
Veterans also experience deployment‑cycle spikes in substance misuse, including post‑deployment binge‑drinking and prescription opioid use following blast or orthopedic injuries. Since 2018, cannabis misuse has risen after many states legalized use, and the delta‑8 THC loophole poses new monitoring challenges, particularly on military bases.
Common Substances Abused
Alcohol
Alcohol is the most commonly misused substance among veterans. Drinking is often tied to poor coping with stress, isolation or trauma.
1 in 3 veterans met the criteria for alcohol use disorder
65 percent of veterans in addiction treatment report alcohol as their most misused substance.
Opiates
Opioids are frequently prescribed for polytrauma-related pain, especially after combat injuries, while benzodiazepines are sometimes misused to self-medicate PTSD-related insomnia.
30 percent of veterans were binge drinkers
1 in 3 met the criteria for hazardous drinking
Stimulants, Cannabis, & Others
Stimulant misuse reflects the demands of high-tempo operational settings where alertness is critical. Cannabis misuse has also risen with state-level legalization.
Other emerging trends, such as gabapentin abuse, kratom use, and energy drink “stacking,” pose new challenges for providers and complicate toxicology screening., Polysubstance use, also called “cocktailing,” is the mixture of alcohol, opioids, benzos.
3.5 percent of veterans reported using cannabis
1.7 percent reported using illicit drugs other than cannabis.
This can magnify overdose risks and make medical detox significantly more complex.
Risk Factors & Co-Occurring Conditions
Risk Factors & Co-Occurring Conditions
Combat Exposure, PTSD & Moral Injury
Veterans exposed to combat often experience PTSD with symptoms of hyperarousal and intrusive memories. This can drive them to self-medicate with alcohol or sedatives. Neurobiologically, trauma-related cues can activate both amygdala fear circuits and reward pathways, thereby increasing cravings and relapse risk.
Beyond PTSD, moral injury is a deep guilt, shame, or feelings of betrayal over perceived ethical violations and has been linked to heavier drinking patterns than PTSD alone. Moral injury may also reduce willingness to engage in trauma-focused care like exposure therapy.
Integrated treatment improves recovery, leading to a higher abstinence rate and greater cost-effectiveness. Integrated treatment shows greater reduction of PTSD symptoms compared to standard care.
Traumatic Brain Injury (TBI) & Chronic Pain
TBI, especially from blast injuries, disrupts dopaminergic pathways by increasing impulsivity and relapse risk in veterans with substance use disorders.
Greater opioid use is common in managing post-blast chronic pain, which can lead to addiction. However, non-opioid multimodal approaches like nerve blocks, ketamine infusions, and physical therapy have shown promise in reducing opioid misuse.
Ongoing symptoms like headaches, vestibular dysfunction, and fragmented sleep impair cognitive abilities and limit a veteran’s participation in group therapy.
These conditions require an individualized treatment approach. Tailoring treatment plans to veterans with TBI and pain is essential to support continued engagement in therapy and minimize the risk of substance dependency.
Military Sexual Trauma (MST) & Gender-Specific Stressors
Roughly 1 in 3 female veterans and an increasing number of male veterans report experiencing military sexual trauma (MST). Many victims turn to alcohol or drugs to dull flashbacks and intrusive thoughts. Under-reporting is common and is often driven by fears of retaliation or disrupting unit cohesion.
Gender-specific treatment groups improve program retention by offering safer spaces for disclosure and healing. Female hormonal fluctuations can also impact how the body processes medications like naltrexone.
Medications used to treat substance use disorders sometimes require dose adjustments in female patients to maintain treatment effectiveness and reduce relapse risk.
Transition to Civilian Life, Isolation & Stigma
Expiration term of service (ETS) refers to the date marking the end of active duty and the option to reenlist or transition back to civilian life.
The first 12 months carries heightened relapse risk due to the loss of unit identity, employment gaps, and reduced social connections. Many veterans delay seeking help for two to three years because they fear their struggles will be seen as weakness.
This stigma is common among Guard and Reserve members who often lack daily peer support. Peer Navigators, Vet Center outreach, and coordinated VA-Department of Labor Transition Assistance workshops help bridge these gaps by building trust by connecting veterans to early intervention, and easing reintegration into civilian roles.
Levels of Care in Addiction Treatment
Levels of Care in Addiction Treatment
Medical Detox & Stabilization
Veteran-focused detox programs provide 24/7 medical monitoring to manage risks such as seizures and withdrawal-related psychosis. Clinical tools like CIWA for alcohol and COWS for opioids help guide safe taper protocols.
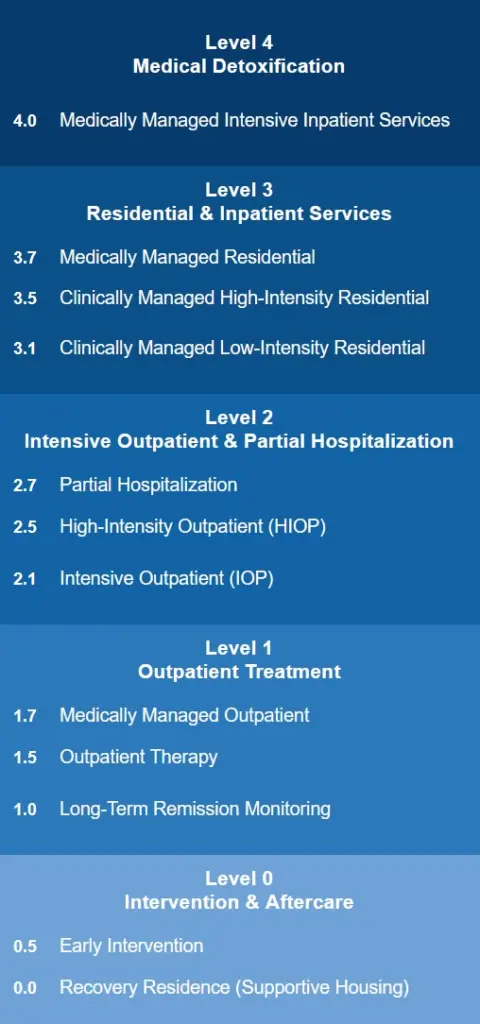
For opioid use, rapid-induction buprenorphine micro-dosing allows smoother transitions from full agonists, minimizing a more dangerous precipitated withdrawal. Medical detox is often the first step in the full levels of care continuum for addiction treatment:
After stabilization, you may receive bridge prescriptions to continue medication-assisted treatment (MAT) in outpatient care. Discharge planning includes dispensing a naloxone kit to reduce the risk of death from overdose during early recovery.
Residential & Inpatient Rehab
Residential addiction treatment programs for veterans like Substance Abuse Residential Rehabilitation Treatment Program (SARRTP) and Domiciliary Care offer trauma-integrated treatment for 28-60 days. Optional housing configurations may include a “squad bay” or private rooms based on gender and MST history.
Care includes daily psychiatric treatment, recreational therapy, and vocational rehabilitation. Some programs include pet therapy, which has demonstrated improvement in mood and engagement.
Facilities follow a zero-tolerance policy for violence and use motivational interviewing rather than punitive measures for relapse. Discharge before completing a program may be triggered by aggression or safety risks.
Partial Hospitalization & Intensive Outpatient Programs
PHP and IOP offer up to six hours per day of outpatient evidence-based group sessions, individual therapy, and skills training. These programs serve as ideal step-down options following inpatient treatment, especially for reservists, working veterans or those managing childcare responsibilities.
Structured but flexible, PHP and IOP emphasize continuity while promoting independence. To support recovery, programs often include random toxicology screens and wearable breathalyzers to improve accountability and early intervention in case of relapse.
Standard Outpatient & VA Telehealth Options
Standard outpatient care combines weekly therapy groups and medication management through VA Video Connect. Veterans complete asynchronous cognitive behavior therapy (CBT) workshops to reinforce coping skills.
Online drug rehab services helps rural veterans avoid travel burdens that can sometimes exceed 200 miles. Urine drug screen kits can be mailed directly to veterans in rehab. Digital platforms track homework and participation, helping clinicians to spot dropout risks early and provide timely support.
Sober Living, Recovery Housing & Transitional Programs
VA Grant & Per Diem-funded sober living offers structured, subsidized housing with veteran-led communities that build accountability and camaraderie. Residents follow mandatory meetings, curfews and receive job search support.
Studies show a 40% higher abstinence rate at 12 months compared to those without recovery housing. Privileges like overnights and curfew extensions are gradually earned, reinforcing stability and progress in early recovery.
Therapies & Treatments Used With Veterans
Therapies & Treatments Used With Veterans
Cognitive Processing Therapy, Prolonged Exposure & EMDR
Cognitive processing therapy (CPT) helps veterans identify and reframe trauma-related “stuck points” via structured workbook homework promoting faster insight. Prolonged exposure techniques use the imagination and real exposures to triggers that reduce avoidance and desensitize trauma triggers.
EMDR therapy uses stimulation to help process fragmented combat memories. EMDR sessions are more effective when veterans first undergo CPT to reduce cognitive resistance. Veterans who first undergo CPT can shorten EMDR sessions by reducing cognitive resistance and identifying trauma-related patterns.
CBT, ACT & Motivational Interviewing
Cognitive behavioral therapy (CBT) helps veterans replace negative automatic thoughts like “I’m broken” with realistic and healthier coping statements. Acceptance and commitment therapy (ACT) encourages accepting intrusive thoughts without judgment and committing to living in line with your values, even during cravings.
Motivational Interviewing (MI) fosters intrinsic motivation through guided “change talk” with a non-confrontational style that predicts higher engagement and successful program completion.
12-Step Facilitation vs. SMART Recovery
Programs like the 12 Steps emphasize spiritual surrender, sponsorship and service. These characteristics are in line with the military’s “battle buddy” ethos of mutual accountability.
In contrast, Self-Management and Recovery Training (SMART) Recovery is secular and grounded in rational emotive behavior therapy (REBT) and CBT and appeals to veterans who may prefer a data-driven model.
Many programs offer dual-track options for veterans to “test-drive” both approaches, which has been shown to improve retention and engagement.
Family & Couples Modalities (FCT, CRAFT)
Family-centered therapy (FCT) builds skills in assertive communication and boundary-setting with added parenting modules tailored for reservists who are balancing service and family life.
Community Reinforcement and Family Training (CRAFT) empowers veterans’ loved ones to reinforce sobriety and avoid enabling. These approaches increase engagement and improve family cohesion.
Mindfulness, Yoga, Meditation & Biofeedback
Mindfulness-based stress reduction (MBSR) lowers cortisol and C-reactive protein levels, which are indicators of inflammation and can improve sleep. Practices like Yoga Nidra and iRest are DoD-endorsed for addressing PTSD-related insomnia. Many units commonly integrate 20-minute recordings into barracks routines.
Heart rate variability, biofeedback and neurofeedback provide real-time tracking of the autonomic nervous system recovery. Veterans use these tools to monitor progress and sustain emotional stability.
Adventure, Equine & Service-Dog-Assisted Therapy
Experiential therapies like rock climbing, paddling and ruck marches help veterans rebuild mastery, restore trust and re-engage the brain’s dopamine system. Service-dog partnerships reduce hypervigilance and offer tactile interruption during cravings, supporting emotional regulation and relapse prevention.
Equine-assisted therapy strengthens sensitivity to non-verbal cues and boundary-setting. Many MST survivors report increased feelings of safety using equine-assisted therapy.
Physical Training, Nutrition & Sleep Optimization
Progressive physical training (PT) reverses deconditioning after detox and boosts mood by engaging the endocannabinoid system. Anti-inflammatory diets rich in omega-3s support gut repair and reduce dysbiosis, which may help to reduce cravings.
Cognitive behavioral therapy for insomnia (CBT-I) and blue-light hygiene help reset circadian rhythms to improve sleep quality. Restorative sleep is essential for neuroplasticity and long-term recovery.
VA, DoD & Community Resources
VA, DoD & Community Resources
VA Substance Use Disorder (SUD) Program Locator & Vet Centers
Veterans can search over 200 SARRTP facilities and 1,000+ community-based outpatient clinics (CBOCs) by ZIP code, with call-center triage enabling same-day detox referrals. You can also filter the directory at Rehab.com for “veterans programs” and the accepted insurance providers.
Vet Centers provide after-hours counseling and family sessions without requiring proof of VA enrollment. For rural veterans, Beneficiary Travel reimbursements and Disabled American Veterans (DAV) vans help overcome transportation barriers and improve access to timely substance use care.
Non-Profit & Private “Veterans-Only” Facilities
Organizations like Wounded Warrior Project (WWP), Home Base, and Project Healing Waters offer grant-funded programs for uninsured veterans. Some private rehab centers feature military-specific tracks with staff members certified as NAADAC Military Addiction Specialists.
When exploring options, veterans should verify that providers have trauma-focused credentials and deliver adequate evidence-based treatment hours per week to ensure clinical quality and personalized care.
Confidentiality, Command Notification & Career Concerns
SUD records are protected under HIPAA and 42 CFR Part 2. Written consent is required for release. “Safe Harbor” self-referral policies allow service members to seek help without facing punitive action.
In 2021, the Brandon Act was signed into law and empowers active-duty service members to request a mental health evaluation. Post-treatment outcomes may lead to limited duty assignments or, in some cases, administrative separation, depending on the determination of a military readiness board.
Paying for Veterans Drug Rehab
Paying for Veterans Drug Rehab
Eligibility for VA Health Benefits & Disability Compensation
VA priority groups determine copay requirements. Many combat-era veterans qualify as Priority 6 and incurring minimal or no fees. Veterans with a service-connected SUD rating are typically exempt from copays and may qualify for travel reimbursement.
For those entering inpatient rehab, VA disability compensation can help offset lost civilian income, providing financial stability during the recovery process.
TRICARE Coverage Tiers (Active-Duty vs. Retiree)
Active-duty service members receive full TRICARE coverage for addiction treatment. There are no out-of-pocket costs regardless if care is provided at a military treatment facility or an authorized civilian center as long as treatment is approved by their command. This includes inpatient detox, outpatient therapy, and MAT.
In contrast, retirees and their dependents are responsible for cost-sharing, but expenses are capped annually at $3,500 under TRICARE’s catastrophic cap.
Prescription medications, including those for substance use and mental health, are typically filled through ExpressScripts’ mail-order delivery service. It’s important to note that treatment authorizations reset at the start of each fiscal year, so beneficiaries should reapply at least 30 days in advance to prevent lapses in coverage.
Private Insurance, Grants & Scholarships
Many private insurance plans cover veteran addiction treatment under mental health parity laws, although deductibles and prior authorization may apply.
Nonprofit organizations and foundations may offer grants and scholarships to cover costs for uninsured or underinsured veterans, especially for programs without VA affiliation. Veterans should inquire about sliding-scale options, state block grants and military-specific aid to significantly reduce financial barriers.
What to Expect From Drug Rehab
What to Expect From Drug Rehab
Pre-Admission Assessments & Required Documentation
Before admission, veterans should gather key documents: DD-214, CAC/ID card, insurance card, medication list, prior behavioral health records and any relevant imaging CDs to support admission and treatment.
An ASAM-based biopsychosocial assessment guides decisions on level of care, detox medications and needed accommodations. A rapid toxicology screen, TB test, and COVID vaccination status help determine safe placement in cohort housing during treatment.
Typical Daily Schedule in a Veteran Residential Program
A structured day begins with 0600 PT formation, 0730 chow, 0900 group therapy, 1100 skills labs and 1400 individual counseling sessions. Evenings include peer support groups, journaling, and recreational activities like woodshop or art therapy, with lights out at 2200.
Weekends feature family-education sessions and off-site AA or SMART Recovery meetings to help veterans build lasting support beyond the treatment setting.
Discharge Planning & Relapse-Prevention Blueprint
Discharge planning begins on day one with an aftercare coordinator assigned to arrange follow-up care before the veteran exits the program.
Each veteran receives a naloxone kit, a personalized relapse trigger list, a crisis-line wallet card and a service-animal plan if needed. A written relapse-prevention plan is shared with consent from a sponsor or family member and is reinforced with a 48-hour post-discharge check-in call.
Life After Rehab
Life After Rehab
Aftercare: VA/Community Outpatient, Tele-IOP & Peer Mentorship
After rehab, veterans can enter an IOP for 90 days through a CBOC or Vet Center via hybrid models that blend in-person and telehealth group sessions.
Tele-IOP platforms use encrypted apps to maintain operational security (OPSEC), and rural veterans can mail saliva samples for compliance testing. Peer mentors, often program alumni, help boost attendance, with incentives like coffee vouchers and gym passes to reinforce ongoing engagement.
Sober Peer Networks (VFW, American Legion, Recovery Apps)
VFW Posts offer peer support groups at local posts by providing local areas for veterans to connect and support each other. Online platforms like RallyPoint, Military OneSource and Vets4Warriors provide ways for veterans to connect in real time.
Programs use buddy-check SMS reminders to reduce relapse spikes tied to holidays, deployment anniversaries, and loss-related dates by offering consistent peer support during high-risk periods.
Employment & Education Resources (VR&E, GI Bill)
VA Vocational Rehabilitation & Employment (VR&E) offers pathways like apprenticeships, supported employment and small-business grant planning for veterans in recovery.
The GI Bill housing allowance helps stabilize finances during early sobriety, while Re-Entry Employment supports re-entry into the workforce. Employers hiring veterans may qualify for the Work Opportunity Tax Credit and the Department of Labor’s HIRE Vets Medallion. These programs encourage recovery-friendly workplaces.
Managing Chronic Pain Without Opioids
VA Whole Health clinics use an integrative approach to pain by bundling whole-person and complementary strategies to reduce reliance on opioids.
For refractory pain, options may include spinal cord stimulation, stellate ganglion blocks and ketamine infusions, when clinically appropriate. Programs can adopt a functional restoration model to focus on life participation at work, relationships and mobility, rather than aiming for complete pain elimination.
Frequently Asked Questions
Frequently Asked Questions
The VA can cover private rehab through the Community Care Network (CCN) when VA facilities are unavailable or too far. Veterans request a consult, and a VA provider submits a CCN referral. Once approved by a third-party administrator, the private facility bills VA directly. Veterans pay only applicable copays, if any.
Yes. Self-referral is protected under the Limited Use Policy, and medical details are shared only on a need-to-know basis.
A command-directed evaluation may lead to temporary duty restrictions, but not automatic discharge. Documenting treatment progress and completing the program successfully is often viewed positively in evaluations and can support long-term career retention.
Most veteran inpatient rehab programs last 28-35 days, although veterans with dual diagnoses or chronic pain may stay 60 days or more.
Duration depends on ASAM criteria, clinical progress, and insurance approval, which does not follow a fixed 30-day model. Many veterans transition to a PHP or IOP for continued structure without hospitalization.
If you relapse, it may signal that your relapse prevention plan needs to be revised or reinforced. Next steps typically include contacting your sponsor, attending an emergency group, and notifying your case manager.
VA Rapid Access clinics or detox readmission can be arranged within 24 hours. Relapse is not failure. It’s treated as clinical data to adjust your care plan and reinforce coping strategies moving forward.
Find Veterans Rehab Near You
Find Veterans Rehab Near You
Looking for veteran-focused addiction treatment?
Use our treatment center directory at Rehab.com to search by location, level of care, insurance accepted, and specialized programs, such as trauma-informed or dual-diagnosis care. Resources are available regardless of whether you’re seeking inpatient rehab, outpatient therapy or transitional housing.
Not sure where to start? Call the number below to speak with someone about your treatment options and verify your insurance coverage for rehab services.
Call A Treatment Provider
For a conversation about what treatment options are available to you.
Make a Call
Addiction Centers That Have Military Programs
Finding facilities near you…

